Practice Policies & Patient Information
Access to your Health Records
Subject Access Requests
A request by a patient, or a request by a third party who has been authorised by the patient, for access under the GDPR (and DPA 2018) is called a Subject Access Request (SAR). If you want to see your health records, or wish a copy, please complete a Practice Subject Access Request Form which you can complete online or please contact the Practice and we will provide you with our paper format. Contact will, subsequently, be made by the Practice to arrange a time for you to come in and collect or read them. You don’t have to give a reason for wanting to see your records and there is no charge for this service. You willl however be required to produce proof of identity before being allowed to read them.
The Practice has up to 28 days to respond to your request. If additional information is needed before copies can be supplied, the 28-day time limit will begin as soon as the additional information has been received.
The 28 day time limit can be extended for two months for complex or numerous requests where the data controller (usually your Practice) needs more time to collate and supply the data. You will be informed about this within 28 days and provided with an explanation of why the extension is necessary.
When writing/calling, you should say if you:
- want a copy of your healthcare records as well as to see them (if you wish to see them your Doctor or member of staff will be present to assist you and explain any medical terms to you)
- want all or just part of them
- would like your records to be given to you in a specific format that meets your needs, and we will endeavour to accommodate your request
- If you request your records to be emailed, then we will secure you or your representative’s agreement (in writing or by email) that they accept the risk of sending unencrypted information to a non-NHS email address
You may also need to fill in an Application Form and give proof of your identity. The Practice has an obligation under the GDPR and DPA2018 to ensure that any information provided for the patient can be verified.
Please note we never send original medical records because of the potential detriment to patient care should these be lost
Who may apply for access?
1(1) Patients with capacity
Subject to the exemptions listed in paragraph 1(6) (below) patients with capacity have a right to access their own health records via a SAR. You may also authorise a third party such as a Solicitor to do so on your behalf. Competent young people may also seek access to their own records. It is not necessary for them to give reasons as to why they wish to access their records.
1(2) Children and young people under 18
Where a child is competent, they are entitled to make or consent to a SAR to access their record.
Children aged over 16 years are presumed to be competent. Children under 16 in England, Wales and Northern Ireland must demonstrate that they have sufficient understanding of what is proposed in order to be entitled to make or consent to an SAR.However, children who are aged 12 or over are generally expected to have the competence to give or withhold their consent to the release of information from their health records. In Scotland, anyone aged 12 or over is legally presumed to have such competence. Where, in the view of the appropriate health professional, a child lacks competency to understand the nature of his or her SAR application, the holder of the record is entitled to refuse to comply with the SAR. Where a child is considered capable of making decisions about access to his or her medical record, the consent of the child must be sought before a parent or other third party can be given access via a SAR (see paragraph 1 (3) below)
1(3) Next of kin
Despite the widespread use of the phrase ‘next of kin’, this is not defined, nor does it have formal legal status. A next of kin cannot give or withhold their consent to the sharing of information on a patient’s behalf. As next of kin they have no rights of access to medical records. For parental rights of access, see the information above.
1(4) Solicitors
You can authorise a Solicitor acting on your behalf to make a SAR. We must have your written consent before releasing your medical records to your acting Solicitors. The consent must cover the nature and extent of the information to be disclosed under the SAR (for example, past medical history), and who might have access to it as part of the legal proceedings. Where there is any doubt, we may contact you before disclosing the information. (England and Wales only – should you refuse, your Solicitor may apply for a court order requiring disclosure of the information. A standard consent form has been issued by the BMA and the Law Society of England and Wales. While it is not compulsory for Solicitors to use the form, it is hoped it will improve the process of seeking consent).
The Practice may also contact you to let you know when your medical records are ready. If your Solicitor is based within our area, then we may ask you to uplift them and deliver them to your Solicitor. This is because we can no longer charge for copying and postage, so we would appreciate your help if you can do this, or alternatively ask your Solicitor if they can uplift your medical records.
1(5) Supplementary Information under SAR requests
The purposes for processing data
The purpose for which data is processed is for the delivery of healthcare to individual patients. In addition, the data is also processed for other non-direct healthcare purposes such as medical research, public health or health planning purposes when the law allows.
The categories of personal data
The category of your personal data is healthcare data.
The organisations with which the data has been shared
Your health records are shared with the appropriate organisations which are involved in the provision of healthcare and treatment to the individual. Other organisations will receive your confidential health information, for example Digital or the Scottish Primary Care Information Resource (SPIRE) or research bodies such as the Secure Anonymised Linkage Databank (SAIL). (This information is already available to patients in our Practice privacy notices).
The existence of rights to have inaccurate data corrected and any rights of objection
For example, a national ‘opt-out’ model such as SPIRE etc.
Any automated decision including the significance and envisaged consequences for the data subject
For example, risk stratification.
The right to make a complaint to the Information Commissioner’s Office (ICO)
1(6) Information that should not be disclosed
The GDPR and Data Protection Act 2018 provides for a number of exemptions in respect of information falling within the scope of a SAR. If we are unable to disclose information to you, we will inform you and discuss this with you.
1(7) Individuals on behalf of adults who lack capacity
Both the Mental Capacity Act in England and Wales and the Adults with Incapacity (Scotland) Act contain powers to nominate individuals to make health and welfare decisions on behalf of incapacitated adults. The Court of Protection in England and Wales, and the Sheriff’s Court in Scotland, can also appoint Deputies to do so. This may entail giving access to relevant parts of the incapacitated person’s medical record, unless health professionals can demonstrate that it would not be in the patient’s best interests. These individuals can also be asked to consent to requests for access to records from third parties.
Where there are no nominated individuals, requests for access to information relating to incapacitated adults should be granted if it is in the best interests of the patient. In all cases, only information relevant to the purposes for which it is requested should be provided.
1(8) Deceased records
The law allows you to see records of a patient that has died as long as they were made after 1st November 1991.
Records are usually only kept for three years after death (in England and Wales GP records are generally retained for 10 years after the patient’s death before they are destroyed).
Who can access deceased records?
You can only see that person’s records if you are their personal representative, administrator or executor.
You won’t be able to see the records of someone who made it clear that they didn’t want other people to see their records after their death.
Accessing deceased records
Before you get access to these records, you may be asked for:
- proof of your identity
- proof of your relationship to the person who has died
Viewing deceased records
You won’t be able to see information that could:
- cause serious harm to your or someone else’s physical or mental health
- identify another person (except members of NHS staff who have treated the patient), unless that person gives their permission
- If you have a claim as a result of that person’s death, you can only see information that is relevant to the claim.
1(9) Hospital Records
To see your Hospital records, you will have to contact your local Hospital.
1(10) Power of attorney
Your health records are confidential, and members of your family are not allowed to see them, unless you give them written permission, or they have power of attorney.
A lasting power of attorney is a legal document that allows you to appoint someone to make decisions for you, should you become incapable of making decisions yourself.
The person you appoint is known as your attorney. An attorney can make decisions about your finances, property, and welfare. It is very important that you trust the person you appoint so that they do not abuse their responsibility. A legal power of attorney must be registered with the Office of the Public Guardian before it can be used.
If you wish to see the health records of someone who has died, you will have to apply under the Access to Medical Records Act 1990. You can only apply if you:
- are that person’s next of kin, are their legal executor (the person named in a will who is in charge of dealing with the property and finances of the deceased person),
- have the permission of the next of kin or have obtained written permission from the deceased person before they died.
- To access the records of a deceased person, you must go through the same process as a living patient. This means either contacting the Practice or the Hospital where the records are stored.
If you think that information in your health records is incorrect, or you need to update your personal details (name, address, phone number), approach the relevant health professional informally and ask to have the record amended. Some Hospitals and GP Surgeries have online forms for updating your details. If this doesn’t work, you can formally request that the information be amended under the NHS complaints procedure.
All NHS trusts, NHS England, CCGs, GPs, Dentists, Opticians and Pharmacists have a complaints procedure. If you want to make a complaint, go to the organisation concerned and ask for a copy of their complaints procedure.
Alternatively, you can complain to the Information Commissioner (the person responsible for regulating and enforcing the Data Protection Act), at:
The Information Commissioner’s Office (ICO)
Wycliffe House,
Water Lane,
Wilmslow,
Cheshire,
SK9 5AF
Telephone: 01625 545745
If your request to have your records amended is refused, the record holder must attach a statement of your views to the record.
Accessible Information Standard
By 31st July 2016 all NHS organisations were required to meet the Accessible Information Standard. This Standard is aimed at making sure that people with disabilities have access to information that they can understand, and receive any communication support they might need.
As part of this initiative, we want to get better at communicating with our patients. If you find it hard to read our letters or if you need someone to support you at appointments, please let us know. We are keen to hear from you if you have a visual or hearing impairment or another disability and would prefer to receive information in any of the following formats.

Please tell us if you, or someone you know, has particular communication needs or requirements that are not shown here, and we will do our utmost to assist.
Benzodiazepine Use For Fear Of Flying
Hadrian Health Centre – Practice Policy
Requests for Benzodiazepines for the indication of Fear of Flying
At Hadrian Health Centre, our practice stance is not to prescribe any Benzodiazepines for the indication Fear of Flying
Reasoning behind this:
In flight Safety:
- Benzodiazepines can cause CNS depression which slows thinking and reaction times. This can increase the risk to the passenger if they are unable to act in an emergency situation, which could put them at a significant risk of not being able to save their life.
- According to the BNF, benzodiazepines can (although uncommonly) cause agitation, which could increase the risk to other passengers and staff.
- Although the medical advice is not to drink alcohol alongside benzodiazepines, the reality is this may not be followed, and cause adverse effects.
VTE risk
- As benzodiazepines have the potential to cause CNS depression, there is an increase risk of developing DVT/PE, which can be fatal. According to research, benzodiazepines have the potential of inducing non-REM sleep which is where a person does not move in their sleep. If a flight is 4 hours or more and the person does not move in this time because they are in this type of sleep, then this further increases their VTE risk
CNS Depressant Effect
- Benzodiazepines have sedating effects, which can cause oxygen saturations to decrease. This is dangerous as oxygen saturation levels are already reduced at altitude.
Law in Other Countries
- In some countries, benzodiazepines are illegal and a patient risks breaking the law if found to be carrying this. Also in some countries where it is illegal, passengers will need to consider the return flight home/onward journey and will need an alternative way of coping with flying
- GPs are only indemnified for medicines administered within the UK.
NICE Guidance Stance
- We should not be prescribing benzodiazepines for mild or self-limiting mental health problems and are only advised for short term use in a crisis in generalised anxiety disorder. For this indication, a person would not be fit to fly. Fear of flying is not generalised anxiety disorder.
BNF
- Phobia is listed as a contraindication for prescribing Benzodiazepines.
Alternative Signposting
- A number of airlines offer information or courses on Fear of Flying via the internet – it could be suggested to the patient to contact their airline provider to see if this is offered but to warn their may be an associated cost to them.
- EasyJet – Fear of flying course | Fearless Flyer (easyjet.com)
- British Airways – Flying with Confidence | Special assistance | British Airways
- Virgin Atlantic – Tips For Nervous Flyers | Advice For Nervous Flyers | Virgin Atlantic
Patient Information Leaflet – Benzodiazepine Use For Fear Of Flying
Care Data
NHS England is currently involved in developing a modern information system, to help improve health services.
To discover how information about you helps us to provide better care you can visit nhs.uk/caredata
Chaperones
Our Practice is committed to providing a safe, comfortable environment where patients and staff can be confident that best practice is being followed at all times; the safety of everyone is of paramount importance.
All medical consultations, examinations and investigations are potentially distressing. Patients can find examinations, investigations or photography involving the breasts, genitalia or rectum particularly intrusive (these examinations are collectively referred to as ‘intimate examinations’). Consultations involving dimmed lights, the need for patients to undress or intensive periods of being touched may also make a patient feel vulnerable.
Chaperoning is the process of having a third person present during such consultations to provide support, both emotional and sometimes physical, to the patient, to provide practical support to the Doctor as required, and also to protect the Doctor against allegations of improper behaviour during such consultations.
Clinical Governance
Clinical governance is the system through which NHS organisations are accountable for continuously improving the quality of their services and safeguarding high standards of care, by creating an environment in which clinical excellence will flourish.
Clinical governance encompasses quality assurance, quality improvement and risk & incident management.
Clinical Research
Clinical Trials help Doctors understand how to treat a particular disease or condition. It may benefit you, or others like you, in the future.
If you take part in a Clinical Trial, you may be one of the first people to benefit from a new treatment.
However, if you do take part you should also be aware that there is a chance that the new treatment turns out to be no better, or worse, than the existing standard treatment.
Complaint Policy
1.1 Introduction
If you have a complaint or concern about the service you have received from the doctors or any of the staff working at Hadrian Health Centre, please let us know. This includes Primary Care Network staff working as part of our GP surgery. We operate a complaints procedure as part of an NHS system for dealing with complaints. Our complaints system meets national criteria.
1.2 How to complain
We hope that most problems can be sorted out easily and quickly when they arise and with the person concerned. For example, by requesting a face-to-face meeting to discuss your concerns.
If your problem cannot be sorted out this way and you wish to make a complaint, we would like you to let us know as soon as possible. By making your complaint quickly, it is easier for us to establish what happened. If it is not possible to do that, please let us have details of your complaint:
- Within 6 months of the incident that caused the problem; or
- Within 6 months of discovering that you have a problem, provided this is within 12 months of the incident.
Complaints should be addressed to the Practice Manager/Deputy Manager verbally or in writing to Hadrian Health Centre, Elton Street East, Wallsend, NE28 8QU. Alternatively, you may ask for an appointment with the GP surgery to discuss your concerns. Please be as specific as possible about your complaint.
1.3 What we will do
We will acknowledge your complaint within three working days. We will aim to have investigated your complaint within 28 working days of the date you raised it with us. We will then offer you an explanation or a meeting with the people involved, if you would like this. When we investigate your complaint, we will aim to:
- Find out what happened and what went wrong.
- Make it possible for you to discuss what happened with those concerned, if you would like this.
- Make sure you receive an apology, where this is appropriate.
Identify what we can do to make sure the problem does not happen again.
If it is not possible to complete our investigation within 28 working days of the date you raised it with us, we will contact you with an updated timescale.
1.4 Complaining on behalf of someone else
We take medical confidentiality seriously. If you are complaining on behalf of someone else, we must know that you have their permission to do so. A letter of consent signed by the person concerned will be needed unless they are incapable (because of illness) of providing this.
1.5 Complaining to NHS England
We hope that you will use our Practice Complaints Procedure if you are unhappy. We believe this will give us the best chance of putting right whatever has gone wrong and an opportunity to improve our GP surgery.
However, if you feel you cannot raise the complaint with us directly, please contact NHS England. You can find more information on how to make a complaint at https://www.england.nhs.uk/contact-us/complaint/complaining-to-nhse/.
1.6 Unhappy with the outcome of your complaint?
If you are not happy with the way your complaint has been dealt with by the GP surgery and NHS England and would like to take the matter further, you can contact the Parliamentary and Health Service Ombudsman (PHSO). The PHSO makes final decisions on unresolved complaints about the NHS in England. It is an independent service which is free for everyone to use.
To take your complaint to the Ombudsman, visit the https://www.ombudsman.org.uk/ or call 0345 015 4033
1.7 Need help making a complaint?
If you want help making a complaint, HealthWatch NorthTyneside can help you find independent NHS complaints advocacy services in your area. Please call 0191 263 5321 or visit www.healthwatchnorthtyneside.co.uk
Patient Advice and Liaison Service (PALS) offer information, advice and support to patients with questions or concerns about an NHS service. Please call 0800 0320202
Confidentiality
You have a right to know who holds personal information about you. This person or organisation is called the Data Controller. In the NHS, the Data Controller is usually your local NHS Board and your GP Surgery. The NHS must keep your personal health information confidential. It is your right.
Please be aware that our staff are bound to the NHS code of confidentiality; they are therefore not permitted to discuss any of our patient’s medical history, including their registration status, without their written consent to do so.
Once written consent has been received and verified with the patient we can provide you with information as required; this includes communicating with you on behalf of the patient with regards to any complaints, but excludes patients who are unable to act on their own behalf and already have a designated person or carer responsible for their medical care.
We therefore respectfully ask parents, relatives and guardians not to request information regarding their relatives/friends or to complain on their behalf unless we have their written consent that you may do so. If consent is required we advise that the person concerned attends the Practice to complete the required form.
Consent Protocol
Consent to treatment is the principle that a person must give permission before they receive any type of medical treatment, test or examination and is generally requested on the basis that an explanation of the required treatment, test or procedure has been received from a Clinician.
Consent from a patient is needed regardless of the procedure, whether it’s a physical examination, organ donation or something else.
The principle of consent is an important part of medical ethics and international human rights law.
Defining consent
For consent to be valid, it must be voluntary and informed, and the person consenting must have the capacity to make the decision.
These terms are explained below:
- voluntary– the decision to either consent or not to consent to treatment must be made by the person themselves, and must not be influenced by pressure from medical staff, friends or family
- informed– the person must be given all of the information in terms of what the treatment involves, including the benefits and risks, whether there are reasonable alternative treatments, and what will happen if treatment doesn’t go ahead
- capacity– the person must be capable of giving consent, which means they understand the information given to them and they can use it to make an informed decision
If an adult has the capacity to make a voluntary and informed decision to consent to or refuse a particular treatment, their decision must be respected.This is still the case even if refusing treatment would result in their death, or the death of their unborn child.
If a person doesn’t have the capacity to make a decision about their treatment, the Healthcare Professionals treating them can go ahead and give treatment if they believe it’s in the person’s best interests.
Clinicians must however take reasonable steps to seek advice from the patient’s friends or relatives before making these decisions.
Read more about assessing the capacity to consent.
How consent is given
Consent can be given:
- verbally– for example, by saying you are happy to have an X-ray
- in writing– for example, by signing a Consent Form for surgery to be performed
Someone could also give non-verbal consent, as long as they understand the treatment or examination about to take place – for example, holding out an arm for a blood test.
Consent should be given to the Healthcare Professional directly responsible for the person’s current treatment, such as:
- a Nurse arranging a blood test
- a GP prescribing new medication
- a Surgeon planning an operation
If someone is going to have a major medical procedure such as an operation, their consent should ideally be secured plenty of time in advance, so that they have time to obtain information about the procedure and ask questions.
If a patient changes their mind at any point before the procedure, they are entitled to withdraw their previous consent.
Consent from children and young people
If they’re able to, consent is usually given by patients themselves. However, someone with parental responsibility may need to give consent for a child up to the age of 16 to have treatment.
Read more about the rules of consent applying to children and young people.
When consent isn’t needed
There are a few exceptions when treatment may be able to go ahead without the person’s consent, even if they’re capable of giving their permission.
It may not be necessary to obtain consent if a person:
- requires emergency treatment to save their life, but they’re incapacitated (for example, they’re unconscious) – the reasons why treatment was necessary should be fully explained once they’ve recovered
- immediately requires an additional emergency procedure during an operation – there has to be a clear medical reason why it would be unsafe to wait to obtain consent, and it can’t be simply for convenience
- with a severe mental health condition such as schizophrenia, bipolar disorder or dementia, lacks the capacity to consent to the treatment of their mental health (under the Mental Health Act 1983) – in these cases, treatment for unrelated physical conditions still requires consent, which the patient may be able to provide, despite their mental illness
- requires Hospital treatment for a severe mental health condition, but self-harmed or attempted suicide while competent and is refusing treatment (under the Mental Health Act 1983) – the person’s nearest relative or an approved Social Worker must make an application for the person to be forcibly kept in Hospital, and two Doctors must assess the person’s condition
- is a risk to public health as a result of rabies, cholera or tuberculosis (TB)
- is severely ill and living in unhygienic conditions (under the National Assistance Act 1948) – a person who is severely ill or infirm and is living in unsanitary conditions can be taken to a place of care without their consent
Consent and life-sustaining treatments
A person may be being kept alive with supportive treatments – such as lung ventilation – without having made an advance decision based on information which outlined the care that they may have refused to receive.
In these cases, a decision about continuing or stopping treatment needs to be made based on what that person’s best interests are believed to be.
To help reach a decision, the Healthcare Professionals responsible for the person’s care should discuss the issue with the relatives and friends of the person receiving the treatment.
They should consider, among other things:
- what the person’s quality of life will be if treatment is continued
- how long the person may live if treatment is continued
- whether there’s any chance of the person recovering
Treatment can be withdrawn if there’s an agreement that continuing treatment isn’t in the person’s best interests.
The case will be referred to the Courts before further action is taken if:
- an agreement can’t be reached
- a decision has to be made on whether to withdraw treatment from someone who has been in a state of impaired consciousness for a long time (usually at least 12 months)
It’s important to note the difference between withdrawing a person’s life support and taking a deliberate action to make them die. For example, injecting a lethal drug would illegal.
Complaints
If you believe you’ve received treatment you didn’t consent to, you can make an official complaint, please write to the Practice Manager, who will assist you with this process.
Data Sharing
For more information about this visit NHS Digital
As of 1st July 2021 your data will be shared with NHS Digital to help improve health, care and services
Patient data from GP medical records kept by GP practices in England is used every day to improve health, care and services through planning and research, helping to find better treatments and improve patient care. The NHS is introducing an improved way to share this information – called the General Practice Data for Planning and Research data collection.
NHS Digital will collect, analyse, publish and share this patient data to improve health and care services for everyone. This includes:
- informing and developing health and social care policy
- planning and commissioning health and care services
- taking steps to protect public health (including managing and monitoring the coronavirus pandemic)
- in exceptional circumstances, providing you with individual care
- enabling healthcare and scientific research
Any data that NHS Digital collects will only be used for health and care purposes. It is never shared with marketing or insurance companies.
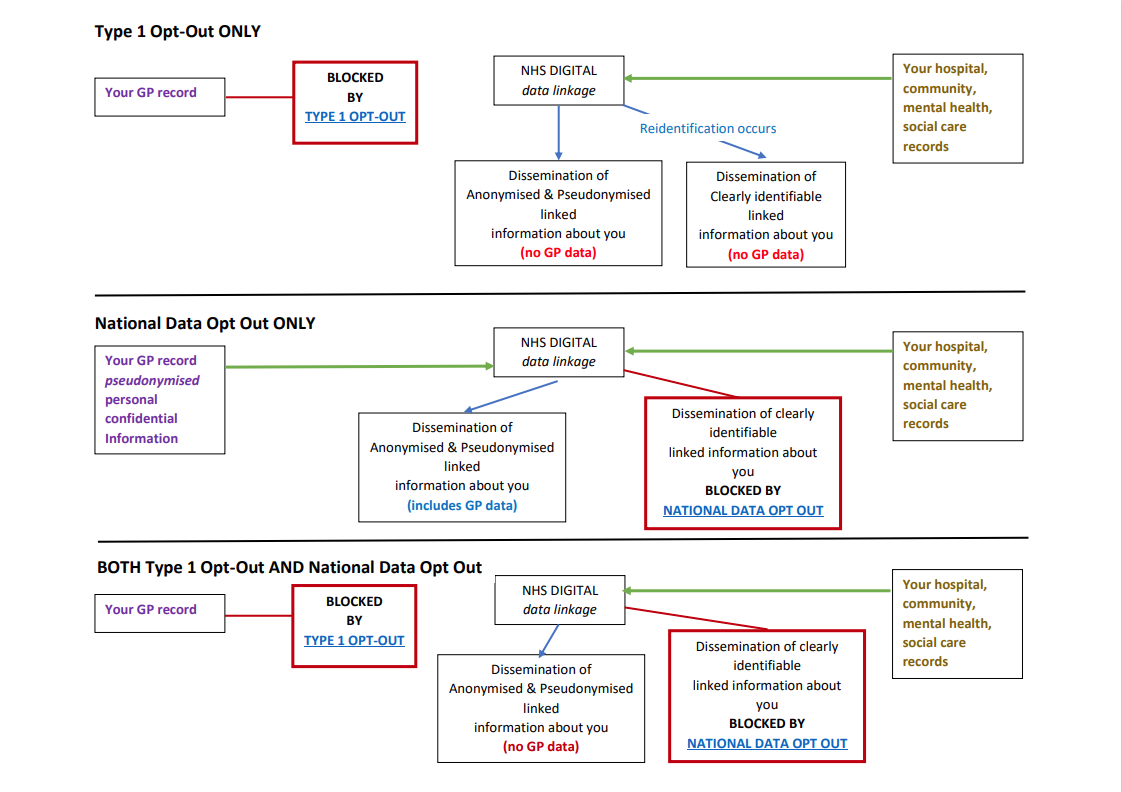
NHS Digital will not collect any patient data for patients who have already registered a Type 1 Opt-out in line with current policy. If this changes patients who have registered a Type 1 Opt-out will be informed.
If you do not want your patient data shared with NHS Digital, you can register a Type 1 Opt-out with us. You can register a Type 1 Opt-out at any time. You can also change your mind at any time and withdraw a Type 1 Opt-out.
Data sharing with NHS Digital will start on 1st July 2021 – please note that this date was postponed on 8th June 2021 – commencement date currently awaited.
If you have already registered a Type 1 Opt-out with your GP practice your data will not be shared with NHS Digital.
If you wish to register a Type 1 Opt-out with your GP practice before data sharing starts with NHS Digital, this should be done by returning this form to us by 1st September 2021 to allow time for processing it. If you have previously registered a Type 1 Opt-out and you would like to withdraw this, you can also use the form to do this. You can send the form by post to us or email it to us at: receptionist.a87029@nhs.net
If you register a Type 1 Opt-out after your patient data has already been shared with NHS Digital, no more of your data will be shared with NHS Digital. NHS Digital will however still hold the patient data which was shared with us before you registered the Type 1 Opt-out.
If you do not want NHS Digital to share your identifiable patient data with anyone else for purposes beyond your own care, then you can also register a National Data Opt-out (also known as Type 2 Opt out).
What do you need to do?
If you are happy for your data to be shared as above, and haven’t previously Opt’d out – you do not need to do anything.
Type 1 OPT-OUT – to stop sharing your details with NHS digital (or to opt back in, if you have previous opt’d out)
Complete this form OPT OUT FORM (or you can complete this to opt back in)
If you are not able to complete this form, call 0300 303 5678 for a form to be posted to you or come into the practice and we can give you a copy to complete.
Then, either;
- Hand the form into reception
- post it to us to: Park Road Medical Practice, 93 Park Road, Wallsend, Tyne & Wear NE28 7LP
- email – receptionist.a87029@nhs.net
Type 2 OPT-OUT (Also known as National Data Opt-out) – If you do not want NHS Digital to share your identifiable patient data with anyone else for purposes beyond your own care, which has been already shared with them (or to opt back in, if you have previous opt’d out)
NOTE: You can only do this via the following ways – as a GP practice we cannot opt you out of Type 2 (National Data Opt-out)
You need to, either;
- Call 0300 303 5678
- or, complete the online form via YOUR NHS MATTERS
Disability Access
If you have any special needs please let our staff know so that we can help you, and also ensure you get the same support in the future. The surgery at Park Road has ramp access. Ground & 1stfloor consulting and treatment rooms are available. Please let staff know if you’re unable to manage the stairs and they’ll’ arrange for you to be seen in a ground floor room. Battle Hill access is all on one level with good car parking facilities.
Wheelchair access
The Practice has been specially designed to make it easier for disabled patients to visit; patients also have access to a disabled toilet.
Disabled parking – Blue badge scheme
The Blue Badge Scheme is for people with severe mobility problems. It allows Blue Badge holders to park close to where they need to go. For more information and an Application Form visit your local council office.
Loop system
We have a loop induction system at Reception to assist the hearing impaired. For more information on the loop hearing system visit Hearing Link website.
- British Deaf Association
- British Sign Language Healthy Mind
- Action Hearing Loss
- Royal Association for Deaf People
- National Deaf Children’s Society
Blind/partially sighted
If you or your family members are blind or partially sighted we can give you a CD or large print of our Practice leaflet upon request. Please ask our staff for further information.
For more advice and support for blind people please visit the following websites:
- Royal National Institute of Blind People (RIND)
- Action for Blind People
- blind.org.uk
- Blind in Business
- British Blind Sport
Guide Dogs
Guide dogs are welcome at the Practice but we ask that you be aware of other patients and staff who may have an allergy or fear of dogs. Please visit the guide dog website for further information.
Duty of Candour
We share a common purpose with our partners in health and social care – and that is to provide high quality care and ensure the best possible outcomes for the people who use our services. Promoting improvement is at the heart of what we do. We endeavour to provide a first class service at all times but sometimes things go wrong and our service may fall below our expected levels. In order to comply with Regulation 20 of the Health and Social Care Act 2008 (Regulations 2014) we pledge to:
Entitlement to NHS Treatment
The NHS is the UK’s state health service which provides treatment for UK residents. Some services are free, other have to be paid for. The regulations that govern who can and can’t receive treatment are complex and may change.
If you have any questions relating to entitlement to treatment under the NHS please contact the Practice.
Free Services
GP and Nurse consultations in primary care, treatment provided by a GP and other primary care services are free of charge to all, whether registering as an NHS patient, or as a temporary patient (which is when the patient is in the area for more than 24 hours and less than 3 months).
For secondary care services, the UK’s healthcare system is a residence based one, which means entitlement to free healthcare is based on living lawfully in the UK on an approved and settled basis. The measure of residence that the UK uses to determine entitlement to free NHS healthcare is known as ‘ordinary residence’. This requires non-EEA nationals subject to immigration control, to also have the immigration status of ‘indefinite leave to remain’. Individuals who are not ordinarily resident in the UK may be required to pay for their care when they are in England. However, some services and some individuals are exempt from payment.
The following NHS treatment is available to anyone:
- Treatment in an emergency (but not follow up treatment)
- Treatment of certain communicable diseases
- Compulsory psychiatric treatment
GPs are the first point of contact for virtually all NHS patients:
- They can direct you to other NHS services and are experts in family medicine, preventative care, health education, and treating people with multiple and long-term conditions
- If you’re planning to live and work in England, you need to register with a local GP
- Being registered with a GP Practice does not in itself mean you’ll be entitled to free NHS hospital treatment
- You’ll need to fill out a GMS1 form (PDF, 156kb) using exactly the same details you used when you filled out your visa
- If you’re in England for a short visit but need to see a GP, you can register as a temporary patient with a local Doctor – to do this, you need to be in the area for more than 24 hours but less than 3 months
- Treatment will be free of charge, but make sure you present your European Health Insurance Card (EHIC) if you have one
Medical emergencies
If you need immediate medical assistance (e.g. because of an accident) telephone 999. The call is free. An Operator will ask you which emergency service you require (Fire, Police or Ambulance). You will need to tell the emergency services what has happened and where you are. If someone is injured and needs to go to Hospital, an ambulance will be sent out to pick the patient up and take them to the nearest Hospital that has an Accident & Emergency Department.
If you need urgent treatment but are well enough to travel please make your own way to the nearest Accident & Emergency Department.
Equality and Diversity
Our Policy is designed to ensure and promote equality and inclusion, supporting the ethos and requirements of the Equality Act 2010 for all visitors to our Practice. We are committed to: If you feel discriminated against: The Practice will not tolerate any form of discrimination or harassment of our staff by any visitor. Any visitor who expresses any form of discrimination against or harassment of any member of our staff will be required to leave the Practice premises immediately. If the visitor is a patient they may also, at the discretion of the Practice Management, be removed from the Practice list if any such behaviour occurs.
Procedure
Discrimination by the Practice or Visitors / patients against you
Discrimination against our Practice staff
Freedom of Information
Anyone has a right to request information from a public authority.
We have two separate duties when responding to these requests:
- to tell the applicant (you or your representative) whether we hold any information falling within the scope of their request; and
- to provide that information
We normally have 20 working days to respond to a request.
For a request to be valid under the Freedom of Information Act it must be made in writing and should be submitted to the Practice Manager and must include the name and address of the applicant, for the reply; the applicant does not need to say why they want the information. Any letter or email to a public authority asking for information is a request for recorded information under the Act.
General Practice Extraction Service (GPES)
General Practice Extraction Service (GPES) is a centrally managed, primary care, data extraction service being introduced across England, and is managed by the Health and Social Care Information Centre (HSCIC). The purpose of GPES is to extract and compare data from across the NHS, allowing data to be turned into accurate and usable management information; this in turn leads to improvements in patient care and greater efficiency across the service as a whole. The data extracted is also used to support QOF, although GPES does not calculate or make these payments, that task is carried out by the Calculating Quality Reporting Service (CQRS). Click on the link below to be redirected to a more in depth review of how ‘Care Data’ is being managed. For further information follow this link.
GP Earnings
The average earnings for the GP’s working in Hadrian Health Centre in the last financial year was £49,652, before taxation and national insurance. This is for 2 full time GP, 17 part time GP’s and 8 locums who worked in the practice for a total of six months or more.
The average earnings reported last year was £54,710
Disclaimer
NHS England require that the net earnings of Doctors engaged in the Practice is publicised, and the required disclosure is shown above. However it should be noted that the prescribed method for calculating earnings is potentially misleading because it takes no account of how much time Doctors spend working in the Practice, and should not be used to form any judgement about GP earnings, nor to make any comparison with any other Practice.
Infection Control Statement
Infection Prevention and Control is the work an organisation does to identify potential risks for spread of infection between patients (and between patients and staff) and to take measures to reduce that risk. The Practice takes its responsibility to do this very seriously.
All staff take responsibility for their own role in this and all staff receive regular training in their role in Infection Prevention and Control.
Medical Research
The practice is a registered Research Ready Practice and we may invite you to be involved in a research study. Research into new treatments and the effectiveness of existing treatments is an essential part of improving the care the NHS gives. All research projects that we are involved with are approved by the National Institute for Health Research. We may receive a payment for arranging a referral into a research programme to cover administration costs. You do not have to accept the offer of participating in a research project.
Named GP Policy
We have allocated a named, accountable GP for all of our registered patients. New patients joining us will be advised of their accountable GP at the point of registration. If you do not know who your named GP is, please ask a member of our Reception Team.
NHS Patient Rights
Citizens Advice England provides patients with a full array of information about your rights within the NHS.
Non-NHS Services
Services which are outwith the NHS Contract
The National Health Service provides most healthcare to the majority of people free of charge, but there are exceptions. GPs are self-employed and are contracted to provide NHS general medical services for their patients.
Sometimes, GPs are asked to provide additional services which fall outside their contract and in these circumstances, they are entitled to make a reasonable charge for providing them.
Your Questions Answered
Isn’t the NHS supposed to be free?
The National Health Service provides most healthcare to the majority people free of charge, but there are exceptions: for example, medical reports for insurance companies.
Surely the Doctor is being paid anyway?
It is important to understand that GPs are not employed by the NHS, they are self-employed and they have to cover their costs – staff, buildings, heating, lighting, etc – in the same way as any small business. The NHS covers these costs for NHS work, but for non-NHS work the fee has to cover the Doctor’s costs.
In recent years, more and more organisations have been involving Doctors in a whole range of non-medical work. Sometimes the only reason that GPs are asked to do non-medical work is because they are in a position of trust in the community, or because an insurance company or employer wants to be sure that information provided is true and accurate.
Examples of non-NHS services for which GPs can charge their NHS patients are:
- accident/sickness insurance certificates
- certain travel vaccinations
- private medical insurance reports
- statements of fact relating to general health e.g. for children’s dance classes
- Letters requested by, or on behalf of, the patient
- Holiday cancellation claim forms
- Referral for private care forms
Examples of non-NHS services for which GPs can charge other institutions are:
- medical reports for an insurance company
- some reports for the DSS/Benefits Agency
- examinations of occupational health
Why does it sometimes take my GP a long time to complete my form?
Time spent completing forms and preparing reports takes the GP away from the medical care of his or her patients. Most GPs have a very heavy workload – the majority work up to 70 hours a week – and paperwork takes up an increasing amount of their time, so many GPs find they have to take some paperwork home at night and weekends.
I only need the Doctor’s signature – what is the problem?
When a Doctor signs a certificate or completes a report, it is a condition of remaining on the Medical Register that they only sign what they know to be true. In order to complete even the simplest of forms, therefore, the Doctor might have to check the patient’s entire medical record. Carelessness or an inaccurate report can have serious consequences for the Doctor with the General Medical Council or even the Police.
What can I do to help?
If you have several forms requiring completion, present them all at once, do not expect your GP to process forms overnight.
Examples of Non-NHS Services include the following:
- Medicals for pre-employment, sports and driving requirements (HGV, PSV etc.)
- Insurance Claim Forms
- Prescriptions for taking medication abroad
- Private Sick Notes
- Vaccination Certificates
The fees charged are based on the British Medical Association (BMA) suggested scales.
| Insurance Companies | |
| a) GP report for insurance applicants | £100.00 |
| b) GP supplementary reports | £30.00 |
| c) Medical examinations undertaken on a GP’s own patient | £110.00 |
| Note: Patients have a right to see the report before it is sent to the insurance company. If a request is made, the insurance company should inform the GP, and the patient has 21 days to arrange to see it. | |
| Note: When an applicant fails to keep a pre-arranged appointment, 50 per cent of the fee should be paid by the insurance company. | |
| Certificates without examination | |
| a) Straightforward certificates of fact | £20.00 |
| More complex certificates | £60.00 |
| Private sick note (incapacity certificate), required by patient for presentation to an employer (except those that the doctor is obliged to provide for statutory sick pay (SSP) purposes) | £15.00 |
| Accident/sickness insurance certificate – short certificate of incapacity without examination for patient to claim under accident/sickness insurance | £60.00 |
| Freedom from infection certificate, eg for school, travel or employment | £15.00 |
| Validation of private medical insurance (PMI) claim form, to support a claim for benefit in connection with private medical insurance, or completion of a ‘pre-treatment’ form | a/b |
| Health club – brief written report to certify that a patient is fit for exercise | £15.00 |
| Passport Forms | £25.00 |
| Work in surgery | |
| a) Extract from records | £56.00 |
| b) Report on a pro forma, no examination (eg 20 minutes) | £110.00 |
| c) Written report without examination, providing a detailed opinion and statement on the condition of the patient (eg 30 minutes) | £110.00 |
| d) Comprehensive clinical examination including report, certificate, or completion of necessary forms (eg 45 minutes) | £150.00 |
| Accident/sickness insurance – to support a claim for payment of benefit under accident/sickness insurance policy | £60.00 |
| Employment – for pre-employment or on an employee, requested by an employer Note: The exception is for local authority employees which are covered |
|
| Miscellaneous Fees | |
| Completion of medical certificate CP3 of the Court of Protection with examination | £138.00 |
| Completion of medical certificate CP3 of the Court of Protection without examination |
£70.00 |
| Serving notice of the Court of Protection (on form CP7) | £70.00 |
| Completion of childminder health form | £90.00 |
| Medical examination of prospective NHS employee – including report and opinion |
£140.00 |
| Report and opinon only of prospective NHS employee | £110.00 |
| Housing Support Letter | £5.00 |
| Fit to attend school/university (no examination) | £15.00 |
| Fit to attend school/university (examination) | £20.00 |
| Work for local authorities | |
| Children in care, adoption & fostering Examinations and reports on children committed, or about to be committed, to the care of a local authority, or received or about to be received into care by a local authority, or about to be fostered |
|
| Initial examination | £75.00 |
| Subsequent examination by the same doctor, or partner, assistant or locum | £25.00 |
| Freedom from infection certificate only | £25.00 |
| Examinations and reports in a form recommended by the British Association for Adoption and Fostering (BAAF) and included in the collaborative arrangements. | |
| Forms C, D, YP or AME (detailed medical examinations to report on child | |
| Forms C, D, YP or AME (detailed medical examinations to report on child | £90.00 |
| Form AH – health assessment on prospective carer | £90.00 |
| Form AH – health assessment on prospective carer | £90.00 |
| Form AH2 – update review from GP records | £90.00 |
| Form IHA – initial health assessment for looked after children | £90.00 |
| Form M & B – obstetric/neo natal report | £90.00 |
| Central Government Departments & Agencies | |
| Criminal injuries compensation authority – GP Report on pro forma | £45.00 |
| Employment Medicals & Reports | |
| HGV Medical – if paid by the patient | £90.00 |
| HGV Medical – if paid by the employer | £165.00 |
| PSV Medical – if paid by the patient | £90.00 |
| PSV Medical – if paid by the patient | £90.00 |
| Taxi Medical – if paid by the patient | £80.00 |
| Taxi Medical – if paid by the employer | £165.00 |
Patient Advice and Liaison Service PALS
The Patient Advice and Liaison Service (PALS) offers confidential advice, support and information on health-related matters. They provide a point of contact for patients, their families and their carers.
Privacy Notice
Please click the link below to see our Privacy Notices below:
Hadrian HC – Privacy Notice – 13.02.2025
Hadrian HC – Children’s Privacy Notice – 13.02.2025
Quality Assurance
Our Practice aims to provide quality, consistent primary care for all patients. We strive to meet the high standards expected in any clinical setting and we expect all members of our Team to work to these standards to help us achieve our aim.
The policies, systems and processes in place in our Practice reflect our professional and legal responsibilities and follow recognised standards of good practice. We evaluate our Practice on a regular basis, through audit, peer review and patient feedback and monitor the effectiveness of our quality assurance procedures.
Quality standards and procedures
To assist our Team in providing our patients with care of a consistent quality we will:
- Provide a safe and welcoming environment
- Ensure all members of our Team are appropriately trained
- Provide patients with information about the Practice and the care available, and ensure the patient understands the terms under which care is offered
- Explain all treatment options and agree clinical decisions with the patient(s), explaining the possible risks involved with each option
- Obtain valid consent for all treatment
- Refer to Specialists for investigation or treatment as appropriate and without undue delay
- Maintain contemporaneous clinical records with an up-to-date medical history for all patients
- Provide secure storage of patients records to main confidentiality
- Explain the procedure to follow for raising a complaint about the service, identifying the Practice contact
To provide our patients with a Team that provides care of a consistent quality we will:
- Provide a safe working environment through hazard identification and risk assessment
- Provide relevant training for all new Team members
- Provide Job Descriptions and Contracts of Employment
- Agree terms for all non-employed contractors working at the Practice
- Maintain staff records, ensuring they are kept as up-to-date as possible
- Ensure staff are notified where all Practice policies and procedures are stored and accessed
Registration Policy
Anyone in England can register with a GP surgery. You do not need proof of address or immigration status, ID or an NHS number. No documents are required to register with a GP; however, to facilitate the registration process we would be happy to see forms of identification and address but if you do not have these – don’t worry!
Documentation may be useful to confirm your details with our local Health Authority which helps to ensure the correct matching of your details to any existing NHS record, enabling previous medical records to transfer smoothly between practices. We appreciate your assistance in this matter.
If you are unable to provide any documentation, then we may still register you. However we may need to contact our Registration Department first, to verify your information with them, and ensure your medical records are not delayed in being transferred to the Practice. This will normally involve a phone call between you, our Registration Department and ourselves. Alternatively we may also email/write to them directly in which case we will require your consent for us to do so.
Further information on How to Register with a GP Surgery is provided by the NHS
If you have any questions regarding NHS entitlement, or our Registration Policy please contact the Practice.
Removal of Patients from our List
It is our policy not to remove patients without serious consideration. If a patient has a serious continuing medical condition, removal will be postponed until the patient’s condition stabilises.
Possible grounds for consideration of removal include:
- Physical violence to staff, Doctors or other patients
- Threat of violence to staff, Doctors or other patients
- Abusive or disruptive behaviour including when under the influence of alcohol or drugs
- Theft from the Surgery, staff, Doctors or other patients
- Criminal damage to the Surgery
- Dangerous dogs posing a real or potential hazard on home visits
- Altering documents e.g. prescriptions, insurance certificates
- Defamation of Doctors or staff
- Misuse of appointments
- Misuse of home visits
- Moving outwith the area
- Any other breakdown of the bond of trust between Doctor and patient
It should be noted that if a patient does not attend for their appointment they will not be given another one for 48 hours. In the event of a patient not attending on three occasions they will receive a letter advising them that if they miss another appointment, they will be removed from our Practice list.
In some cases we reserve the right to remove other members of the household. We will continue to be responsible for the patient’s medical care for a period of up to 8 days from the date of notification to our local health authority or until the patient registers with another Doctor, whichever is the sooner.
Patient information leaflet: Removal from our list
Safeguarding
Safeguarding Children
Our Primary Care Team is committed to safeguarding children. The safety and welfare of children who come into contact with our services either directly or indirectly is paramount, and all staff have a responsibility to ensure that Best Practice is followed, including compliance with statutory requirements.
We are committed to a Best Practice which safeguards children and young people irrespective of their background, and which recognises that a child may be abused regardless of their age, gender, religious beliefs, racial origin or ethnic identity, culture, class, disability or sexual orientation.
The Primary Care Team are committed to working within agreed policies and procedures and in partnership with other agencies, to ensure that the risks of harm to a child or young person are minimised. This work may include direct and indirect contact with children, access to patient’s details and communication via email or text message/telephone.
Our Surgery is supported by the CCG who have designated Nurses and Doctors in post who offer professional expertise and advice regarding safeguarding children.
Safeguarding Vulnerable Adults
The practice holds regular safeguarding meetings. If you have a concern about the safety or welfare of a vulnerable adult in North Tyneside, First Call is the first point of contact for everybody to use. Telephone: 0191 643 2777
Monday to Friday, 08:30 – 17:00.
In an emergency, outside of these times ring: 0300 123 0812
A copy of the practice policy can be viewed here – Safeguarding Vulnerable Adults.
Shared Decision Making
Making decisions about your care with your doctor or nurse (shared decision making)
When you visit your doctor’s surgery you will often find that there are decisions to be made about your health and the treatments that might be available to you. This includes when you are choosing between different types of treatment or different ways of managing any condition(s) you have. When these decisions are made it is important that you are part of that process, so that you are able to come to the best decisions based on what is important to you.
Shared Decision Making
Your doctor/nurse is an expert about health and health care. You are an expert in knowing about yourself, the impact that any conditions have on you, and what is important to you in treating your condition and in your wider life. When you and your doctor/nurse work together to share what you both know, and then use all of that information to come to a decision together, this is called ‘Shared Decision Making’.
How to get involved
In order for you to be involved in decisions about your care there are three key things you need to know;
- What are my options?
- What are the possible risks, benefits and consequences of each option?
- How can we make a decision together that is right for me?
With shared decision making your doctor/nurse is there to support you by providing good quality information, helping you understand this information, and giving you support and guidance as you think about what is most important to you. This will help you to understand what choices are available to you, the pros and cons of each option, and then use that information to come to a decision together about the best option for you.
If you would like to know more about Shared Decision Making the following video provides further information.
Where to find more information
Here are some links to information which may help you make any decisions about your healthcare
Patient Decision Aids
Patient Decision Aids (PDAs) are designed to help you decide which treatments and care options are best for you.
PDAs are useful because they allow you to pick out the things that are most important to you (your values) and make comparisons about how different treatments might affect these values. Patient decision aids have been developed for a number of common health care decisions and your doctor/nurse may use one or refer you on to one when you talk with them, or you might find it useful to look at one by yourself. If you would like to know more about patient decision aids and look at some of the patient decision aids that are publicly available, the following websites :
Decision aids developed in the UK
An international inventory of decision aids.
If you are looking for information about the risk of cardio vascular disease or Type 2 diabetes and ways in which those risks can be reduced these sites contains some useful information:
Sharing your Information with Others
Collecting and sharing information is essential to provide safe and effective healthcare. Appropriate information sharing is an essential part of the provision of safe and effective care. Patients may be put at risk if those who provide their care do not have access to relevant, accurate and up-to-date information about them. All staff have an ethical and legal duty to keep patient information confidential. If you do not wish your health information to be shared please notify the Practice in writing, in order that we may update your record.
Summary Care Records (SCR)
Summary Care Records (SCR) are an electronic record of important patient information, created from GP medical records. They can be seen and used by authorised staff involved in a patient’s direct care, both within the Practice as well as in other areas of the healthcare system.
Your Summary Care Record
Care professionals in England use an electronic record called the Summary Care Record (SCR). This can provide those involved in your care with faster secure access to key information from your GP record.
The NHS have produced an information leaflet about SCR; this is available using the link below, to either view or download as you wish.
What is an SCR?
If you are registered with a GP Practice in England, you will already have an SCR unless you have previously chosen not to have one.
It includes the following basic information:
- Medicines you are taking
- Allergies you suffer from
- Any bad reactions to medicines
It also includes your name, address, date of birth and unique NHS Number which helps to identify you correctly.
What choices do you have?
You can now choose to include more information in your SCR, such as significant medical history (past and present), information about management of long term conditions, immunisations and patient preferences such as end of life care information, particular care needs and communication preferences.
Your SCR is available to authorised healthcare staff providing your care anywhere in England, but they will ask your permission before they look at it. This means that if you have an accident or become ill, healthcare staff treating you will have immediate access to important information about your health.
This Practice supports SCR however, as a patient you have a choice:
- If you would like an SCR you do not need to do anything and an SCR will be created for you
- If you do NOT want an SCR please complete the SCR opt out form
Remember, you can change your mind about your SCR at any time. Talk to our Practice if you want to discuss your option to add more information or decide you no longer want an SCR. If you do nothing we will assume you are happy for us to create a SCR for you.
Vulnerable patients and carers
Having an SCR that includes extra information can be of particular benefit to patients with detailed and complex health problems. If you are a carer for someone and believe that this may benefit them, you could discuss it with them and their GP Practice.
Who can see my SCR?
Only authorised, professional healthcare staff in England who are involved in your direct care can have access to your SCR. Your SCR will not be used for any other purposes.
These staff:
- Need to have a Smartcard with a chip and passcode
- Will only see the information they need to do their job
- Will have their details recorded every time they look at your record
Healthcare professionals will ask for your permission if they need to look at your SCR. If they cannot ask you because you are unconscious or otherwise unable to communicate, they may decide to look at your record because doing so is in your best interest. This access is recorded and checked to ensure that it is appropriate.
SCRs for children
If you are the parent or guardian of a child under 16, and feel they are able to understand this information you should show it to them. You can then support them to come to a decision about having an SCR and whether to include additional information. You may request to opt them out of SAR; any opt-out requests on behalf of children will be carefully considered.
Confidentiality
For information on how the NHS will collect, store and allow access to your electronic records visit the NHS website.
Unacceptable Actions Policy
We believe that patients have a right to be heard, understood and respected. We work hard to be open and accessible to everyone. Occasionally, the behaviour or actions of individuals using our Practice makes it very difficult for us to deal with their issue or complaint. In a small number of cases the actions of individuals become unacceptable because they involve abuse of our staff or our process. When this happens we have to take action to protect our staff, and must also consider the impact of the individuals behaviour on our ability to do our work and provide a service to others. This Policy explains how we will approach these situations. People may act out of character in times of trouble or distress. There may have been upsetting or distressing circumstances leading up to us being made aware of an issue or complaint. We do not view behaviour as unacceptable just because a patient is forceful or determined. In fact, we accept that being persistent may sometimes be a positive advantage when pursuing an issue or complaint. However, we do consider actions that result in unreasonable demands on our Practice or unreasonable behaviour towards Practice staff to be unacceptable. It is these actions that we aim to manage under this Policy. We understand that patients may be angry about the issues they have raised with the Practice. If that anger escalates into aggression towards Practice staff, we consider that unacceptable. Any violence or abuse towards staff will not be accepted. Violence is not restricted to acts of aggression that may result in physical harm. It also includes behaviour or language (whether verbal or written) that may cause staff to feel offended, afraid, threatened or abused. We will judge each situation individually, and appreciate individuals who come to us may be upset. Language which is designed to insult or degrade, is derogatory, racist, sexist, transphobic, or homophobic or which makes serious allegations that individuals have committed criminal, corrupt, perverse or unprofessional conduct of any kind, without any evidence, is unacceptable. We may decide that comments aimed not at us, but at third parties, are unacceptable because of the effect that listening or reading them may have on our staff. A demand becomes unacceptable when it starts to (or when complying with the demand would) impact substantially on the work of the Practice. Examples of actions grouped under this heading include: Sometimes the volume and duration of contact made to our Practice by an individual causes problems. This can occur over a short period, for example, a number of calls in one day or one hour. It may occur over the life-span of an issue when a patient repeatedly makes long telephone calls to us, or inundates us with letters or copies of information that have been sent already or that are irrelevant to the issue. We consider that the level of contact has become unacceptable when the amount of time spent talking to a patient on the telephone, or responding to, reviewing and filing emails or written correspondence impacts on our ability to deal with that issue, or with other Patients’ needs. When we are looking at an issue or complaint, we will ask the patient to work with us. This can include agreeing with us the issues or complaint we will look at; providing us with further information, evidence or comments on request; or helping us by summarising their concerns or completing a form for us. Sometimes, a patient repeatedly refuses to cooperate and this makes it difficult for us to proceed. We will always seek to assist someone if they have a specific, genuine difficulty complying with a request. However, we consider it is unreasonable to bring an issue to us and then not respond to reasonable requests. Individuals with complaints about the Practice have the right to pursue their concerns through a range of means. They also have the right to complain more than once about the Practice, if subsequent incidents occur. This contact becomes unreasonable when the effect of the repeated complaints is to harass, or to prevent us from pursuing a legitimate aim or implementing a legitimate decision. We consider access to a complaints system to be important and it will only be in exceptional circumstances that we would consider such repeated use is unacceptable – but we reserve the right to do so in such cases. We have to take action when unreasonable behaviour impairs the functioning of our Practice. We aim to do this in a way that allows a Patient to progress through our process. We will try to ensure that any action we take is the minimum required to solve the problem, taking into account relevant personal circumstances including the seriousness of the issue(s) or complaint and the needs of the individual. Where a patient repeatedly phones, visits the Practice, raises repeated issues, or sends large numbers of documents where their relevance isn’t clear, we may decide to: • limit contact to telephone calls from the patient at set times on set days, about the issues raised • restrict contact to a nominated member of the Practice staff who will deal with future calls or correspondence from the patient about their issues • see the patient by appointment only • restrict contact from the patient to writing only regarding the issues raised • return any documents to the patient or, in extreme cases, advise the patient that further irrelevant documents will be destroyed • take any other action that we consider appropriate Where we consider continued correspondence on a wide range of issues to be excessive, we may tell the patient that only a certain number of issues will be considered in a given period and ask them to limit or focus their requests accordingly. In exceptional cases, we reserve the right to refuse to consider an issue, or future issues or complaints from an individual. We will take into account the impact on the individual and also whether there would be a broader public interest in considering the issue or complaint further. We will always tell the patient what action we are taking and why. When a Practice employee makes an immediate decision in response to offensive, aggressive or abusive behaviour, the patient is advised at the time of the incident. When a decision has been made by Senior Management, a patient will always be given the reason in writing as to why a decision has been made to issue a warning (including the We record all incidents of unacceptable actions by patients. Where it is decided to issue a warning to a patient, an entry noting this is made in the relevant file and on appropriate computer records. Each quarter a report on all restrictions will be presented to our Senior Management Team so that they can ensure the policy is being applied appropriately. A decision to issue a warning to a patient as described above may be reconsidered either on request or on review. It is important that a decision can be reconsidered. A patient can appeal a decision about the issuance of a warning or removal from the Practice list. If they do this, we will only consider arguments that relate to the warning or removal, and not to either the issue or complaint made to us, or to our decision to close a complaint. An appeal could include, for example, a patient saying that: their actions were wrongly identified as unacceptable; the warning was disproportionate; or that it will adversely impact on the individual because of personal circumstances. The Practice Manager or a GP Partner who was not involved in the original decision will consider the appeal. They have discretion to quash or vary the warning as they think best. They will make their decision based on the evidence available to them. They must advise the patient in writing that either the warning or removal still applies or a different course of action has been agreed. We may review the warning periodically or on further request after a period of time has passed. Each case is different. This policy is subject to reviewSection 1 – What actions does the Practice consider to be unacceptable?
Section 2 – Aggressive or abusive behaviour
Section 3 – Unreasonable demands
Section 4 – Unreasonable levels of contact
Section 5 – Unreasonable refusal to co-operate
Section 6 – Unreasonable use of the complaints process
Section 7 – Examples of how we manage aggressive or abusive behaviour
Section 8 – Examples of how we deal with other categories of unreasonable behaviour
Section 9 – Other actions we may take
Section 10 – The process we follow to make decisions about unreasonable behaviour
Section 11 – How we let people know we have made this decision
duration and terms of the warning) or remove them from the Practice list. This ensures that the patient has a record of the decision.Section 12 – How we record and review a decision to issue a warning
Section 13 – The process for appealing a decision
Your Data
Information about your health and care helps us to improve your individual care, speed up diagnosis, plan your local services and research new treatments. The NHS is committed to keeping patient information safe, and will always be clear about how it is used. Information about your individual care such as treatment and diagnoses is collected about you whenever you use health and care services. It is also used to help both the Practice and other organisations for research and planning, for example research into new treatments, deciding where to put GP clinics and planning for the number of Doctors and Nurses in your local Hospital. It is only used in this way when there is a clear legal basis to use the information to help improve health and care for you, your family and future generations. Wherever possible we try to use data that does not identify you, but sometimes it is necessary to use your confidential patient information. You do not need to do anything if you are happy about how your information is used. However, if you do not want your confidential patient information to be used for research and planning, you can choose to opt out securely, either online or through a telephone service. You can change your mind about your choice at any time. No, choosing to opt out will not affect how information is used to support your care and treatment. You will still be invited for screening services, such as screenings for bowel cancer. If you are happy for your confidential patient information to be used for research and planning, you do not need to do anything. To find out more about the benefits of data sharing, how data is protected, or to make/change your opt-out choice visit www.nhs.uk/your-nhs-data-matters You can also view/download the leaflet below for your information.Your Data Matters to the NHS
How your data is used
You have a choice
Will choosing this opt-out affect your care and treatment?
What do you need to do?
Your Rights and Responsibilities
Attending a busy GP Practice as a patient can be an anxious and worrying time for you. We aim to make your time here as short and as simple as possible and the following should help to explain what you, as a patient, can expect from our staff and what we, the staff, can expect from you.
Your Doctor’s Responsibilities
- To treat you with respect and courtesy at all times
- To treat you as an individual, and to discuss with you the care and treatment we can provide
- To give you full information on the services we offer
- To give you the most appropriate care by suitably qualified staff
- To provide you with emergency care when you need it
- To refer you to a suitable Consultant when necessary
- To give you access to your health records, subject to any limitations in the law
Your Responsibilities as a Patient
- To treat all staff with respect and courtesy at all times
- To tell us if you are unsure about the treatment we are offering you
- To ask for a home visit only when you are unable to attend the Practice through illness or infirmity
- To request such a visit before 10.00 am, if possible
- To ask for an out-of- hours visit only when necessary
- Please ensure that you order your repeat medication in plenty of time allowing 48 working hours for your request to be processed
- To keep to your appointment time (note: if you are more than 10 minutes late for your appointment you may not be seen)
- To notify us at least 24 hours prior to an appointment if you cannot attend
- To notify us of any changes to your personal details (e.g. name, address, telephone number, mobile numbers etc).
Zero Tolerance
It is our policy to be helpful and polite to all our patients regardless of age, ethnic origin, disability, gender or sexual orientation. We expect the same courtesy from our patients. Discriminatory, unsocial, threatening, violent or abusive behaviour towards staff, other patients or the premises will not be tolerated.
In England, please refer to NHS Constitution your rights and responsibilities for further information.
As an employer, the Practice has a duty to care for the health and safety of its staff. The practice also has a legal responsibility to provide a safe and secure working environment for staff. All patients are expected to behave in an acceptable manner and violent or abusive behaviour towards staff or patients may result in removal from our practice list or even criminal proceedings. The practice follows the NHS guidance concerning Zero Tolerance.
The NHS operate a Zero Tolerance Policy with regard to violence and abuse and the Practice has the right to remove violent patients from their list with immediate effect, in order to safeguard practice staff, patients and other persons. Violence in this context includes actual or threatened physical violence or verbal abuse which leads to fear for a person’s safety. In this situation we will notify the patient in writing of their removal from the list and record in the patient’s medical records the fact of the removal and the circumstances leading to it.
Where patients are disruptive and display aggressive and/or intimidating behaviour and refuse to leave the premises, staff are instructed to dial 999 for Police assistance, and charges may then be brought against these individuals.
We will not deal with anyone, in anyway, who shouts at us. We will advise you at the time that we cannot deal with you because you are shouting – and we may begin the process of removal from our patient list
The Practice supports the government’s ‘Zero Tolerance’ campaign for Health Service Staff. This states that GPs and their staff have a right to care for others without fear of being attacked or abused. To successfully provide these services a mutual respect between all the staff and patients has to be in place. All our staff aim to be polite, helpful, and sensitive to all patients’ individual needs and circumstances. You are respectfully reminded that it is very often the case whereby staff are simultaneously confronted with a multitude of varying and sometimes difficult tasks and situations.
If you are seriously unhappy with the quality of service you have the right to register with another practice without notifying us. Similarly, on the very rare occasions when a patient repeatedly ignores their responsibilities to the Practice, we have the right to remove the patient from our Practice list.
The practice has the right to remove violent patients from the list with immediate effect in order to safeguard practice staff, patients and other persons. Please note:
- Violence in this context includes actual or threatened physical violence or verbal abuse which leads to fear for a person’s safety. In this situation we will notify the patient in writing of their removal from the list and record in the patient’s medical records the fact of the removal and the circumstances leading to it.
- Intimidation in this context includes shouting or talking in an aggressive or passive-aggressive raised voice; or making inappropriate comments.
- Harassment in this context includes persistent and repeated telephone calls, or face-to-face confrontations, when the definitive answer has already been given and the person to whom you are talking is unable or does not have the authority to satisfy the demands of your request.
The Practice takes it very seriously if a member of staff or one of the doctors or nursing team is treated in an abusive or violent way. Aggressive behaviour, be it violent or abusive, will not be tolerated and may result in you being removed from the Practice list and, in extreme cases, the Police being contacted.
Inappropriate and unacceptable behaviours may include but are not limited to:
- Using threatening or abusive language involving swearing or offensive language at practice staff or other service users
- Any behaviour which we consider intimidating or disruptive
- Excessive noise (e.g. recurrent loud or intrusive conversation or shouting)
- Any physical violence towards any member of the Primary Health Care Team or other patients, such as pushing or shoving
- Racial abuse and sexual harassment will not be tolerated within this practice
- Persistent or unrealistic demands that cause stress to staff will not be accepted. Requests will be met wherever possible and explanations given when they cannot
- Causing damage/stealing from the Practice’s premises, staff or patients
- Obtaining drugs and/or medical services fraudulently
Our Zero Tolerance Policy also covers directing abuse at the Practice and/or Staff via Social Media
- We welcome all feedback as it gives us the opportunity to review the services that we provide and, where necessary or appropriate, make changes or improvements. We encourage patients to feedback to the surgery through appropriate channels and we can then act on it as necessary.
- Feedback is a useful part of the interaction between Hadrian Health Centre and its patients and other service users. However, derogatory, abusive or offensive comments about Hadrian Health Centre or staff on social media are not an acceptable part of the relationship between both parties.
- We have a duty to protect our staff from online abuse.
- Posting derogatory and/or offensive comments online can cause unwarranted distress to our Practice members and Staff and cause patients to delay or dissuade from presenting to the surgery to receive medical treatment
- If any derogatory posts regarding the Hadrian Health Centre or its staff are brought to our attention, they could be viewed as a potential breakdown in the doctor-patient professional relationship and may result in the individual being removed from our list.
- Legal advice will be sought and the appropriate action taken against any patient who posts defamatory comments.
- Defamatory comments about our team are not to be shared on any social media platform.
- We have a separate complaints policy which patients are to use should they wish to make a complaint. We will only respond to complaints made to the Hadrian Health Centre in accordance with the organisation’s policy.
We ask you to treat our staff members courteously at all times.
Thank you.
